
| Non-perforated appendicitis with multiple
appendicoliths, clinical symptoms mimicking psoas muscle
inflammation. 13 year old boy presented with three day history of right lower quadrant pain after weight-lifting which included squats. There was no history of nausea, vomiting, fever, or leukocytosis. On physical examination, positive peritoneal signs (abdominal guarding and rebound tenderness) were elicited. CT examination was performed to evaluate for possible abscess, shown below. |
 |
Figure 1. Axial CT scan through the upper pelvis shows a fluid-filled, dilated appendix (arrowheads) which extends medially from the cecum (C), lying at the anterior aspect of the right psoas muscle (P on the right). The cephalad aspect of a calcified appendicolith is present in the appendiceal neck, shown more completely in the subsequent image (below). Multiple dilated, fluid-filled ileal loops (I) are present, which can result in diagnostic confusion unless the connection of the appendix with the cecum and a distal blind end can be identified. |
 |
Figure 2. CT image just caudal to Figure 1 shows the calcified appendicolith (arrow) obstructing the appendiceal neck. Note multiple dilated ileal loops (I). |
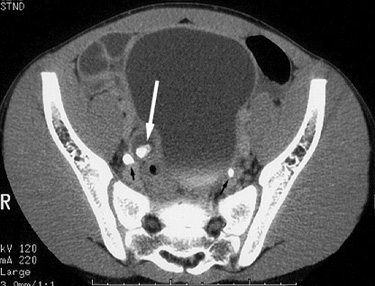 |
Figure 3. CT image at a lower level than Figure 2 shows a second appendicolith (large white arrow)within the fluid-filled dilated appendix. Note the similarity in appearance to the contrast-filled, dilated right distal ureter (small black arrow on the right; small black arrow on the left is the non-dilated distal left ureter). |
 |
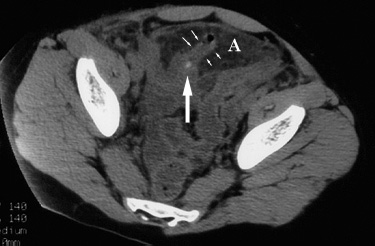
Figure 4. CT scan further caudal than Figure 3 shows the distal right ureter (black arrow) compressed by the adjacent dilated, fluid-filled appendix (A).B = urinary bladder. |
| Surgery revealed acute, non-perforated appendicitis. |
Return to Diagnostic Imaging Overview
Return to CT Technique and Accuracy
Return to CT Findings
Case 2
| Non-perforated appendicitis. 9 year old male who presented to the emergency department with a six hour history of generalized abdominal pain. The patient was febrile, and a complete blood count revealed leukocytosis. CT, shown below, was requested to evaluate for appendicitis. |
 |
Figure 1. Contrast-enhanced CT image at level of the midpelvis shows a dilated, thick-walled appendix (*) with a small amount of adjacent fluid (arrows). |
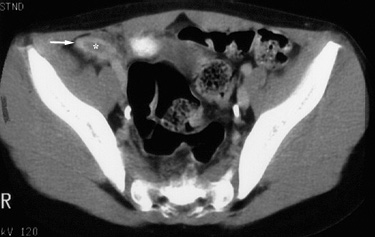 |
Figure 2. Contrast-enhanced CT image, several centimeters inferior to Figure 1, shows the blind-ending tip (arrow) of the dilated, thick-walled appendix (*). |
| At surgery, an inflamed, non-perforated appendix was removed. |
Return to CT Findings
Case 3
| Non-perforated appendicitis. 11 year old female ten days status-post a motor vehicle accident who presented to the emergency room with a concomitant history of intermittent abdominal pain, emesis and fever. The pain had acutely worsened and was exacerbated with walking. Physical examination revealed diffuse abdominal tenderness. Clinical considerations included duodenal hematoma and appendicitis. An upper GI examination was performed the following day which showed lack of flow of barium beyond the jejunum (not shown). The abdominal pain localized to the right lower quadrant and leukocytosis increased. A CT examination, shown below, was then obtained. |
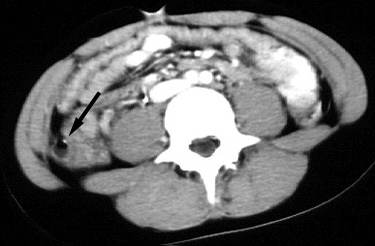 |
Figure 1. Contrast-enhanced CT image through lower abdomen demonstrates a calcified appendicolith (arrow) within the dilated, fluid-filled appendix. |
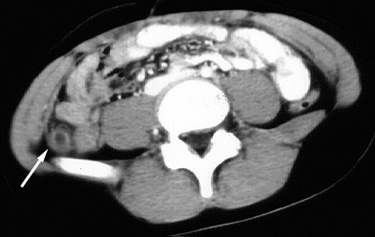 |
Figure 2. Contrast-enhanced CT image through the upper pelvis demonstrates an enlarged appendix (arrow) with infiltration of the surrounding retroperitoneal fat. |
| An inflamed, non-ruptured appendix was found at surgery. |
Return to CT Findings
| Non-perforated appendicitis. 18 year old girl of substantial body habitus presented to the emergency room with a three day history of right lower quadrant pain. A CT examination was performed without oral or rectal contrast, shown below. |
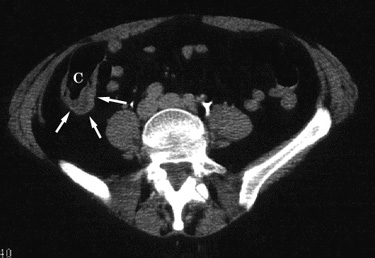 |
Figure 1. Intravenous contrast enhanced CT image through the lower abdomen demonstrates mural thickening (arrows) of the cecum (C) at the base of the appendix, representing the "arrowhead sign" associated with appendicitis. |
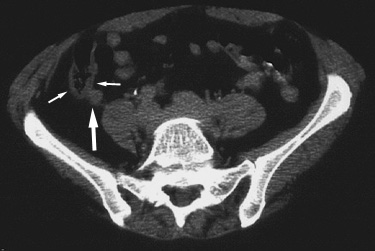 |
Figure 2. CT image obtained slightly caudal to Figure 1 show cecal wall thickening (small arrows) and the adjacent dilated appendix (large arrow). |
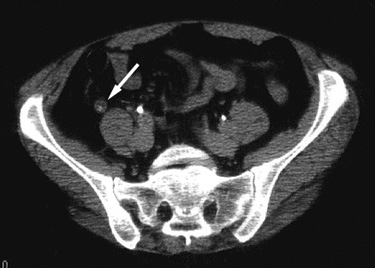 |
Figure 3. CT image at a more caudal level than Figure 2 shows an enlarged appendix which contains an appendicolith (large arrow). Note contrast opacified distal ureters bilaterally (small arrows) |
| At surgery, an inflamed, nonperforated appendix was removed. |
Return to CT Findings
Case 5
| Nonperforated appendicitis. 20 year old boy with history of epigastric pain and vomiting since the morning of his visit to the emergency room. There was no history of fever, chills, sweats, diarrhea or constipation. Clinical diagnosis of appendicitis was considered, and patient was observed in the hospital for one day. Ultrasound (not shown) obtained the next day showed no upper abdomen or right lower quadrant pathology. The appendix was not visualized. Serial physical examinations over the ensuing four hours revealed the pain to have moved from the epigastrium to the right lower quadrant.At this time the leukocytosis had increased from 15,000 WBC / ml to 19,000 WBC/ ml. In light of worsening and shifting abdominal pain, the diagnosis of appendicitis was reconsidered and exploratory laparotomy recommended. However, at this time, the patient refused surgery because the physicians could not guarantee the presence of appendicitis. A CT scan was,therefore, obtained (shown below). |
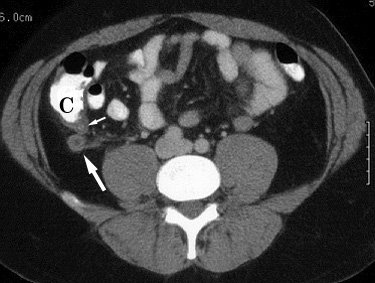 |
Fig 1. CT image just above the pelvic inlet shows thickened wall of the cecum (C) with a calcified appendicolith (small arrow) in the neck of the inflamed appendix (large arrow). |
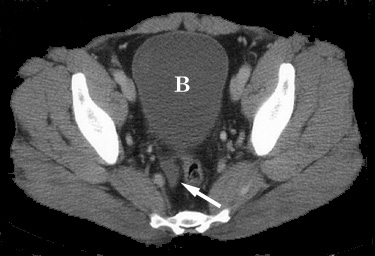 |
Fig 2. A CT scan in the pelvis shows free fluid in the pelvis (arrow) posterior to the bladder (B). |
| At surgery a nonperforated inflamed appendix was removed. The patient was discharged home in good condition on the second postoperative day. |
Return to CT Findings
Case 6
| Perforated appendicitis. 18 year old girl presented at an outside hospital with mid-abdominal pain for two days and was treated with Zantac. She presented to our emergency room four days later with sudden onset of diaphoresis, nausea, vomiting, and loose stools. The patient described a classical history of appendicitis with initial mid-epigastric pain, lasting approximately two days, which shifted to the right lower quadrant. A CT scan was obtained at this time, shown below. |
 |
Intravenous contrast-enhanced CT image of the pelvis demonstrates dilated, fluid-filled appendix (arrow). In this case, rectal contrast was not necessary to differentiate the inflamed appendix from surrounding bowel. |
| At surgery, a necrotic appendix was removed. The adjacent peritoneal fluid was infected, therefore the surgical wound was left open, anticipating a delayed primary closure. The patient's clinical course was further complicated by a wound infection which required intravenous antibiotics. |
Return to CT Findings
| Perforated appendicitis with generalized
peritonitis. 5 year old girl was diagnosed with appendicitis by CT (not shown) after a one day history of right lower quadrant pain.She was treated with oral antibiotics and had scheduled an elective appendectomy for the following week. She now presents three days after the initial CT with nausea, vomiting, fever, and right lower quadrant tenderness. Repeat CT examination was obtained, shown below. |
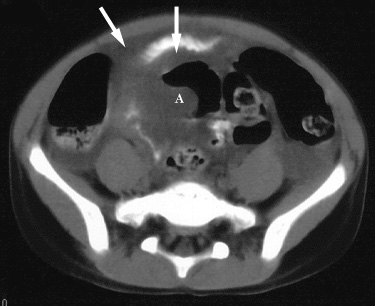 |
Figure 1. CT image through the mid pelvis shows free intraperitoneal fluid (arrows) and displacement of adjacent bowel by an ill-defined abscess (A). |
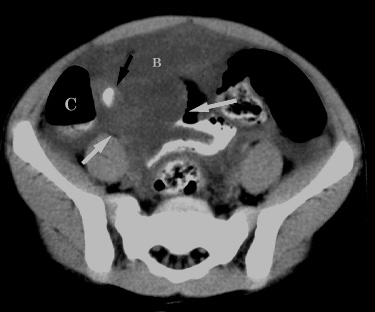 |
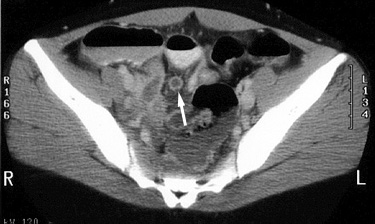
Figure 2. CT image at a level slightly lower than in Figure 1 demonstrates a calcified appendicolith (black arrow) adjacent to the cecum (C). Mass effect caused by the abscess (white arrows) is redemonstrated. Note difficulty in distinguishing non-contrast opacified bowel (B) from surrounding free intraperitoneal fluid. |
| An inflamed, perforated appendix with an adjacent abscess was found at surgery. |
Return to Pathophysiology
Return to Atypical Clinical Presentation (C)
Return to Primary Treatment
Return to CT Findings
| Perforated appendicitis with generalized
peritonitis and multiple abscesses. 14 year old girl presented with one week history of nausea, vomiting, and fever. A CT scan was performed to evaluate for appendicitis, shown below. |
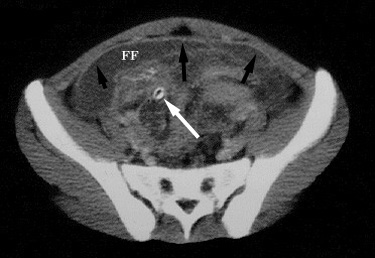 |
Figure 1. Axial CT image in the upper pelvis shows free intraperitoneal fluid (FF) with enhancement of the peritoneum (black arrows) consistent with peritonitis. A calcified appendicolith (white arrow) is present. |
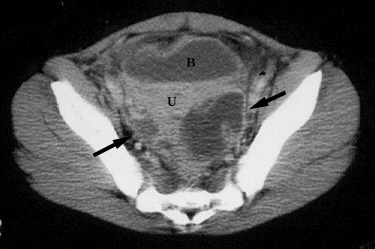 |
Figure 2. CT image lower in the pelvis demonstrates loculated abscess collections (black arrows) posterior to the uterus (U). Bladder (B) is seen anterior to the uterus. |
 |
Figure 3. CT image at a similar level as Figure 1, obtained two weeks later after intravenous antibiotic and fluid therapy, demonstrates interval increase in size of the infected peritoneal fluid collection (A). Note the abnormal enhancement and thickening of the peritoneum (arrow). |
| The right lower quadrant abscess was drained under CT guidance. Despite the drainage and intravenous antibiotic therapy, the patient had persistent fever and subsequently developed pelvic pain two weeks later. Repeat CT scan demonstrated resolution of the initially drained abscess. However, a pelvic cul-de-sac abscess remained, shown below. |
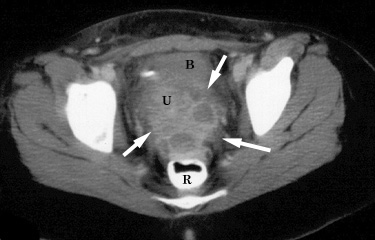 |
Figure 4. CT image at the level of the lower pelvis demonstrates a multiloculated fluid collection with enhancing margins (arrows) representing a low pelvic abscess. The uterus (U) and bladder (B) are seen more anteriorly. Note relationship of the abscess to the rectum (R). This relationship allowed successful ultrasound guided abscess drainage. |
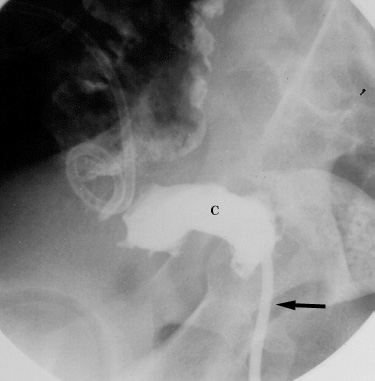 |
Figure 5. Fluoroscopic lateral abdominopelvic image obtained after US guided transrectal placement of catheter (black arrow) into pelvic abscess filled with contrast (C). Pigtail catheter at the right of the image is the initial abscess drainage catheter, subsequently removed. |
Return to Pathophysiology
Return to Atypical Clinical Presentation (C)
Return to CT Findings
Return to Primary Treatment
Return to Treatment of Postoperative Complications
| Perforated appendicitis with an obstructing
appendicolith and a fluid-filled, dilated appendix. 13 year old girl presented with increasing right lower quadrant pain of one day's duration. |
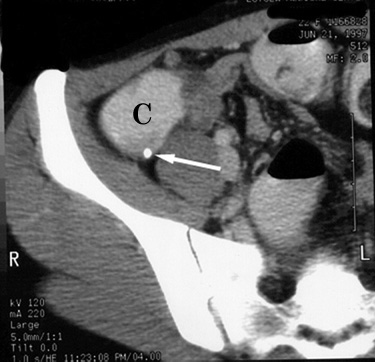 |
Figure 1. Contrast enhanced axial CT image in the upper pelvis demonstrates a calcified appendicolith (arrow) in the region of the appendiceal neck adjacent to the cecum (C). |
 |
Figure 2. CT image obtained caudal to Figure 1 shows a dilated, fluid-filled, obstructed appendix (arrows). Sigmoid colon (S) and rectum (R) are seen posteriorly. |
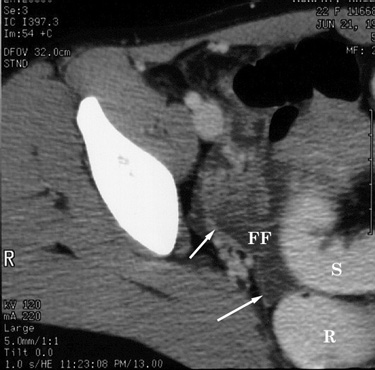 |
Figure 3. CT image obtained slightly caudal to figure 2 shows free fluid (FF) with enhancing peritoneum (arrows). S = sigmoid colon; R = rectum |
| At surgery, a suppurative, perforated appendix was removed. |
Return to Pathophysiology
Return to CT Technique and Accuracy
Return to CT Findings
Case 10
| Perforated appendicitis with pericecal
abscess. 7 year old girl presented to the emergency room with two day history of right lower quadrant pain, fever, and emesis. A CT examination was obtained to evaluate for appendicitis, shown below. |
 |
Intravenous contrast-enhanced CT image of the lower abdomen shows an enhancing retrocecal mass (A) consistent with an abscess. There is inflammatory infiltration (arrows) of the retrocecal fat. |
| The patient was treated with intravenous antibiotics. A repeat CT examination performed three days later demonstrated decrease in the size of the abscess (not shown). Elective appendectomy was perfomed without complications one month later. |
Related teaching points can also be found in Primary Treatment
Return to CT Findings
| Perforated appendicitis with a mildly dilated
appendix. 14 year old girl presented to the emergency room with fever, right lower quadrant pain, and emesis for three days.Laboratory evaluation showed leukocytosis. Plain abdominal radiograph was obtained, shown in Plain Film Findings. CT was also performed to evaluate for appendicitis, discussed in CT Findings section. |
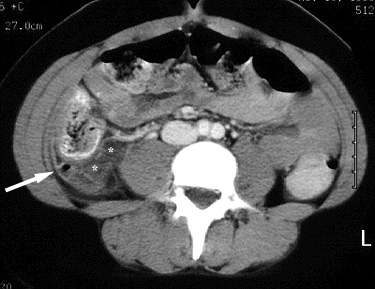 |
Figure 1. Contrast-enhanced CT image at the lower abdominal level shows a mildly dilated appendix which contains an air-fluid level (arrow). There is a small fluid collection (*) just medial to the appendix. |
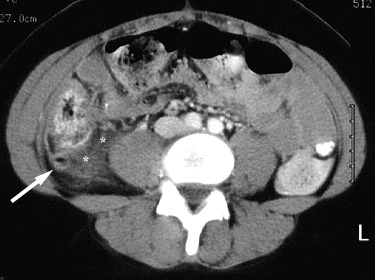 |
Figure 2. Contrast-enhanced CT image at a level just below Figure 1 again shows air and fluid in a mildly dilated and thickened appendix (arrow). There is adjacent periappendiceal infiltration (*). |
| At laparoscopic surgery, there was perforated appendicitis and a small peri-appendiceal abscess. |
Return to CT Findings
| Perforated appendicitis with multiple
abscesses. 3 year old girl with abdominal pain and vomiting for five days was treated at an outside hospital with oral antibiotics.The patient improved slightly but presented to our emergency room two days later with similar symptoms and new leukocytosis. A CT scan was performed, shown below. |
 |
Figure 1. CT image of the upper abdomen shows a subphrenic abscess (arrows). |
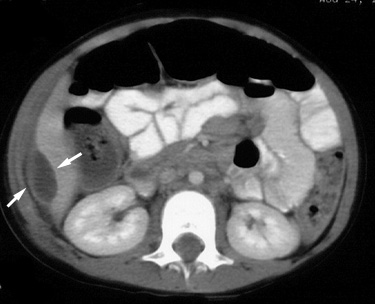 |
Figure 2.. CT scan at a lower level shows a perihepatic abscess (arrows). |
 |
Figure 3. CT image of the lower abdomen shows a multi-loculated fluid collection with enhancing walls consistent with an abscess (arrows). |
 |
Figure 4. Axial CT image at a lower level than figure 3 shows a pericecal abscess with thickened walls (arrows). |
| The pericecal abscess shown in Figure 4 was drained percutaneously with CT guidance. However, because of persistent fever for the following four days, another CT scan was performed. This showed resolution of the paracecal and perihepatic abscesses but increase in the size of the subphrenic abscess (not shown). A second drain was placed in the subphrenic abscess under CT guidance, after which the fever resolved. Elective appendectomy was performed one month later without complications. |
Return to CT Findings
Return to Primary Treatment of Complicated Appendicitis
| Perforated appendicitis with periappendiceal
abscess. 7 year old boy who presented with a one day history of fever, anorexia, emesis and abdominal pain. He was afebrile in the emergency department, but a complete blood cell count revealed leukocytosis. CT, shown below, was requested to evaluate for appendicitis. |
 |
Figure 1. Contrast-enhanced CT image at the level of the iliac crest shows an inflammatory mass (arrows) between the cecum (C) and opacified small bowel (*). If small bowel opacification had been less optimal, the inflammatory mass could have been mistaken for unopacified distal ileum. |
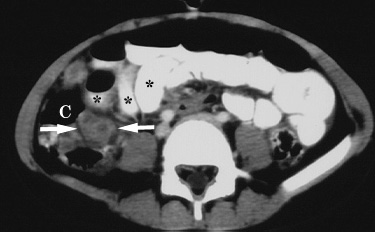 |
Figure 2. Contrast-enhanced CT image 5 mm caudal to Figure 1 also shows the inflammatory mass (arrows) between the cecum (C) and opacified small bowel (*). |
| Surgery confirmed perforated appendicitis with a periappendiceal abscess. |
Return to CT Technique and Accuracy
Return to CT Findings
Case 14
| Perforated appendicitis with interloop
mesenteric abscess. 12 year old girl who presented to the emergency department with a two day history of fever, abdominal pain and emesis. CT, shown below, was requested to evaluate for appendicitis. |
 |
Contrast-enhanced CT image, immediately superior to the iliac crest shows a midline gas and fluid collection consistent with an abscess (A). Note infiltration of adjacent mesenteric fat (*). |
| Because of interloop location, the abscess was not amenable to percutaneous drainage. The patient was brought to the operating room, and perforated appendicitis with abscess was confirmed. |
Return to CT Findings
| Perforated appendicitis. 10 year old girl had been diagnosed with perforated appendicitis and small adjacent abscess by ultrasound (for more details, return to US case presentation). After seven days of intravenous antibiotics, her abdominal pain and fever persisted. A CT examination was obtained for further evaluation. |
 |
Non-contrast enhanced CT image of the pelvis demonstrates the enlarged, inflamed appendix (small arrows), which contains an appendicolith (large arrow), protruding into an anterior abdominal fluid collection representing an abscess (A). |
| The periappendiceal abscess was percutaneously drained using CT guidance. The patient responded well, becoming afebrile and asymptomatic. An elective appendectomy was performed without complications one month later. |
Related teaching points can also be found in Primary Treatment
Return to US Findings
Return to CT Findings