Cerebrovascular disease / Stroke
Objectives: You will learn
- Common causes for stroke
- Optimal imaging procedures to investigate stroke
- Image findings of stroke
- How to read imaging studies when stroke is suspected
Q1: What are the common causes of stroke?
- Ischemic
- due to atherosclerotic disease
- large vessel disease (extracranial, intracranial)
- small vessel disease (intracranial)
- commonly results from an embolus dislodged from an atherosclerotic plaque at the bifurcation of common carotid artery/proximal internal carotid artery
- from inadequate cerebral blood flow due to decreased perfusion pressure
- cardiogenic emboli
- Hemorrhagic
- Venous sinus thrombosis
- Vasculitis (non-atheromatous inflammation), (less common)
- Traumatic arterial dissection (less common)
Q2: Which imaging procedure should be ordered to evaluate stroke?
- CT is the imaging modality of choice to rule out hemorrhagic stroke.
- Evidence of hemorrhage will be a contraindication to the use of thrombolytic or anticoagulant agents.
- MR is the imaging modality of choice for diagnosis of acute stroke.
Q3: What are the advantages and disadvantages of CT?
Advantages:
- Easy access and shorter scanning time. CT brain study can be done in less than one minute, if necessary, particularly in an unstable and uncooperative patient.
Disadvantages:
- It may not detect an acute infarct.
- It has limited capacity to show smaller infarcts in the brain stem, cerebellum, basal ganglia and thalamus.
Q4: What are the advantages and disadvantages of MRI?
Advantages:
- MRI is more sensitive than CT for the early diagnosis of brain infarction.
- DWI (diffusion-weighted pulse sequence) is diagnostic for early detection of acute stroke.
- DWI images are useful in distinguishing acute from chronic ischemic changes.
- MRI can identify sites of old hemorrhage better than CT.
- Brain stem infarcts and small cortical infarcts are seen with higher sensitivity.
Disadvantage:
- Patients who are unstable and claustrophobic patients may not cooperate for the MRI study. Patients with contraindication to MRI (e.g., with pacemaker) need to rely on CT imaging study.
Q5: Does a normal CT rule out stroke?
Q6A: What are the imaging findings of acute infarction (<24 hours) ?
Non-contrast CT:
- Can be normal
- Acute infarction may be seen as hypodense area relative to surrounding normal brain
- Loss of gray-white matter differentiation
- Cortical sulcal effacement
- Blurred basal ganglia
- Insular ribbon sign (blurred insular cortex due to edema)
- Dense MCA sign (hyperdense middle cerebral artery), hyper dense basilar artery due to intra-arterial thrombus
- CT is superior to MRI in detecting hemorrhagic transformation within an infarct (15-45%)
MRI:
- Diffusion weighted imaging (DWI) is the most sensitive MR sequence in detection of acute infarction (95% sensitive).
- The region of acute infarction is seen as an area of bright signal intensity on DWI which can be detected within minutes of acute stroke.
- DWI sequence is sensitive to restricted diffusion within the cell from stroke-induced cytotoxic edema and thus the region of acute stroke is seen as bright signal on DWI. Cytotoxic edema can occur immediately after the initial insult, thus DWI can reveal the area of acute infarction immediately after the insult.
- T2 wtd. flair images may be normal within 4-6 hours of acute stroke. Thus, conventional MR pulse sequences are sensitive in detecting acute stroke by 70-80%, whereas diffusion wtd images (DWI) increases the sensitivity to 95%.
Q6B: What are the imaging findings of subacute stroke (24 hours to 1 week) ?
- Both CT and MR images will demonstrate edema, mass effect without or midline shift (depends upon the size of infarction).
- Cortical gyral enhancement, typical of subacute infarction will be seen in the subacute phase and the enhancement will slowly start disappearing by two months.
- Hemorrhagic transformation of acute stroke can occur during 24-48 hours after the initial insult.
Q6C: What are the imaging findings of subacute to chronic infarction (1 week to 2 months) ?
- Resolution of edema and mass effect.
- Resolution of parenchymal enhancement.
Q6D: What are the imaging findings of chronic old infarct (>2 months) ?
- End result of acute infarct.
- Focal well defined wedge shaped area of low attenuation (with CT density close to fluid) involving a vascular distribution.
- Sulci adjacent to an old infarcted area, enlarge secondary to parenchymal volume loss (encephalomalacia).
- Ventricular enlargement is also seen if the infarcted area is adjacent to the ventricle.
- Residual old blood product may persist (MRI is more sensitive than CT in detecting old hemosiderin blood product.
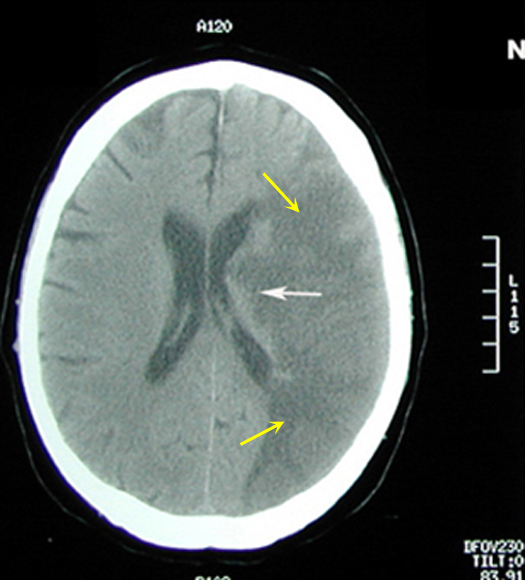
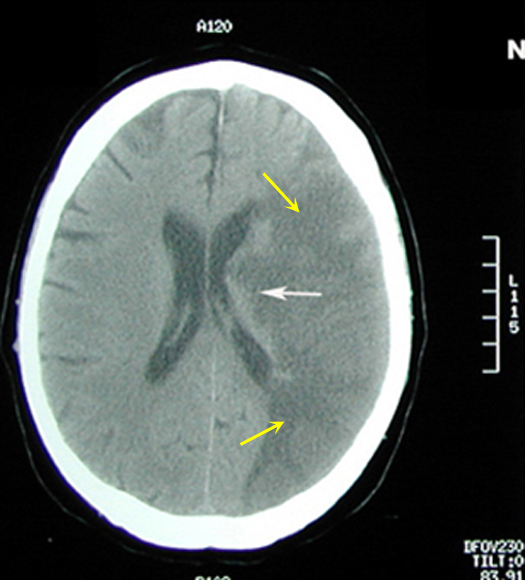
Figure 1: Non-contrast axial CT brain
|
Acute to Subacute Infarct
Case 1:
Imaging findings: Figure 1
- Large area of low CT attenuation (hypodense) is seen involving the left middle cerebral artery distribution (yellow arrows), with involvement of both gray and white matter.
- White arrows points to involvement of basal ganglia region with infarction also.
- Gyri and sulci are effaced on the left side (compare to normal right side).
|
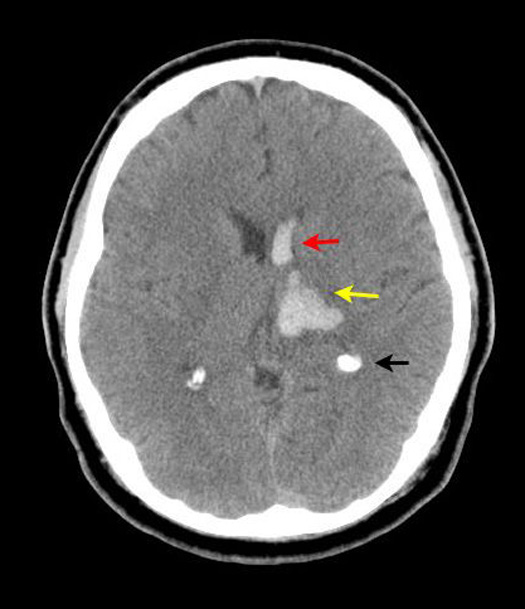
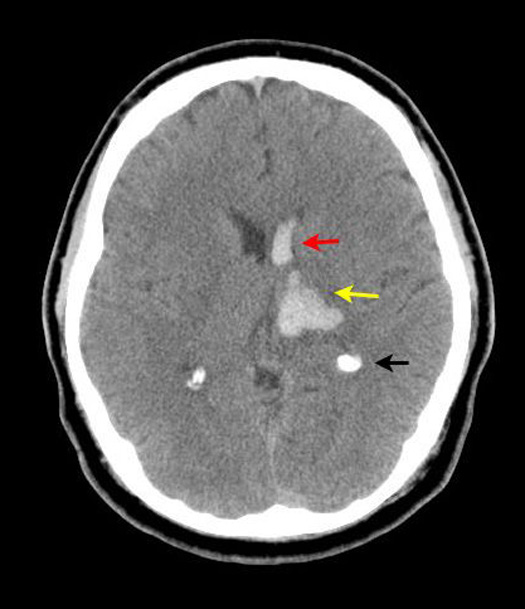
Figure 2: Non-contrast axial CT head
|
Hypertensive Hemorrhagic Infarct
Case 2:
Imaging findings: Figure 2
-
Hemorrhage (hyperdense area) involving left basal ganglia/thalamic regions (yellow arrow) is noted.
-
Extension of hemorrhage into left frontal horn (red arrow).
-
Black arrow points to normal calcification of choroid plexus.
Hemorrhage secondary to hypertension is more common in basal ganglia / thalamic regions.
Not a candidate for thrombolytic therapy or anticoagulation. |
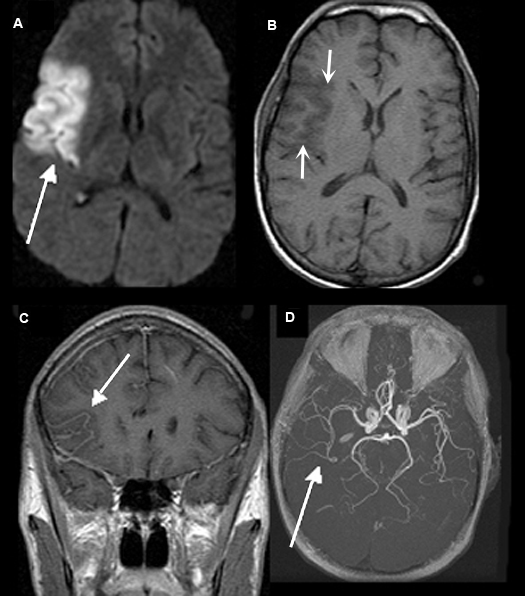
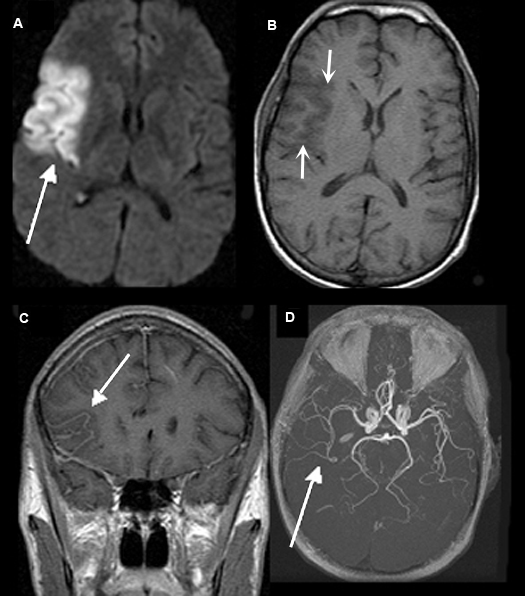
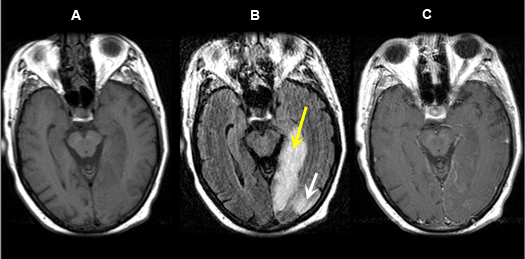
Figure 3: MR Images
|
One Day Old Acute Infarction Involving the Right Middle Cerebral Artery (MCA) Territory
Case 3:
Imaging findings: Figure 3
- Diffusion weighted image identifies an area of acute infarct as bright signal (white arrow).
- Pre-contrast axial T1 wtd.. MRI shows gyral thickening (arrows) compared to contralateral side. Findings of acute infarct are not as readily visible as in DW pulse sequence.
- Post-contrast coronal T1 wtd. MRI shows delayed vascular enhancement (white arrow) in the area of infarct due to distal arterial occlusion.
- MR angiography shows right middle cerebral artery branches to be narrower in caliber (white arrow), as compared to left side, likely from embolic occlusion.
|
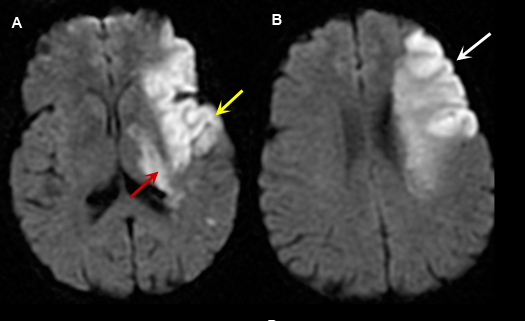
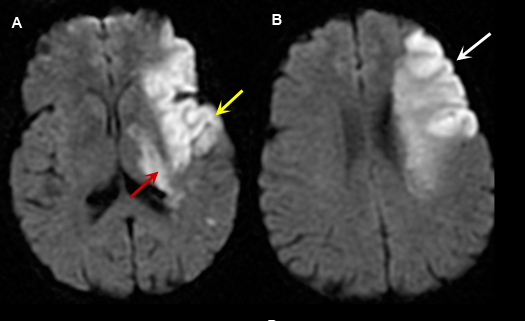
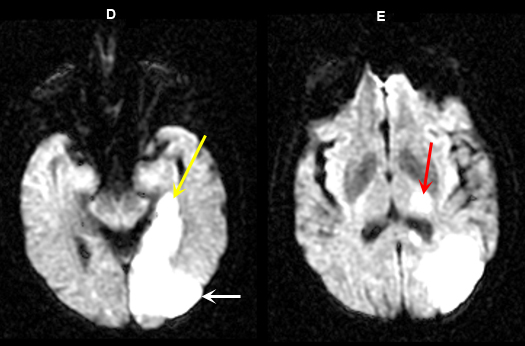
Figure 4: MR Images (DWI)
|
Left Middle Cerebral Artery Territory Acute Stroke
Case 4:
Imaging findings: Figure 4
- A and B: Diffusion weighted images shows areas of acute infarction as bright signal due to intracellular cytotoxic edema, restricting movement of water molecule in and out of the cell.
- In figure A, left temporal lobe acute infarction (yellow arrow) and left lateral basal ganglia-thalamic regions (red arrow) are noted.
- Left frontal lobe infarct (arrow) is shown in Fig. B.
|
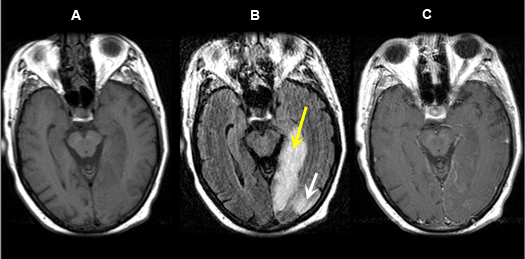
Figure 5 A-C: MR Images
|
Posterior cerebral artery territory Acute Stroke
Case 5:
Imaging findings: Figure 5 A-C
- Pre-contrast axial T1 wtd. MRI
- Axial flair image
- Post-contrast axial T1 wtd. MRI
Acute infarction is seen involving the left occipital lobe (yellow arrow) and adjacent left temporal lobe (white arrow). The left posterior cerebral artery territory infarction is better seen on flair sequence (Fig. B) than on T1 wtd. pulse sequence (Figs. A, C).
|
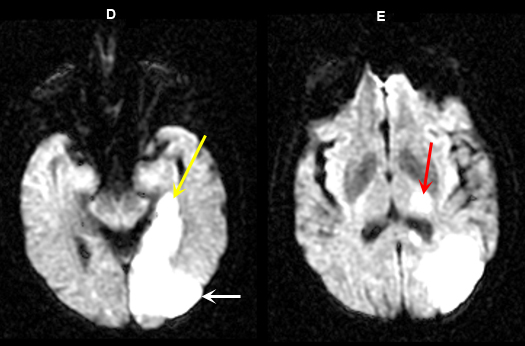
Figure 5 D-E: MR Images
|
Imaging findings: Figure 5 D-E (DW images)
Acute infarction involving the left occipital lobe (yellow arrow in Fig. A), adjacent left temporal lobe (white arrow in Fig. D) and infarction within the left thalamus (red arrow in Fig. E) is best appreciated on diffusion wtd. pulse sequences. |
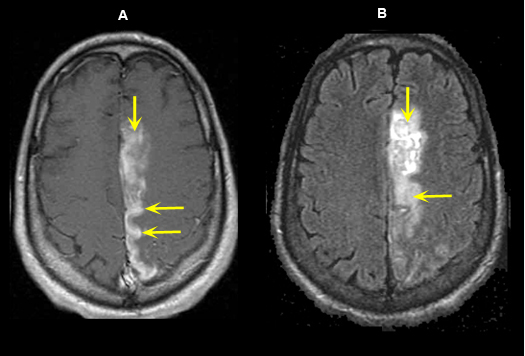
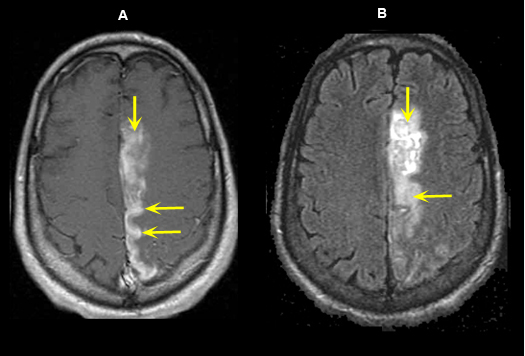
Figure 6: MR Images
|
Left Anterior Cerebral Artery Territory Acute Infarction (5 days old)
Case 6:
Imaging findings: Figure 6
- Post-contrast axial T1 wtd. image demonstrates gyral enhancement (yellow arrows) involving the territory of left anterior cerebral artery.
- Flair image shows an area of increased signal (yellow arrows) related to acute infarct.
|
Q7: Describe possible subsequent changes following acute infarction (See answers to Q6B, 6C, 6D).
When an embolus blocking a major vessel migrates, lyses, or disperses, recirculation into the infarcted area can cause a hemorrhagic infarction and may aggravate edema formation due to disruption of the blood-brain barrier.
- After 24 hours, a cerebral or cerebellar infarct is usually seen as a hypodense area by CT and abnormal signal intensity by MRI involving both the gray and white matter in a typical vascular distribution.
- Whether or not hemorrhagic transformation occurs, a mass effect may develop due to edema and is at its maximum three-five days post infarct (Fig. 7C).
Subacute to chronic infarct: (1-8 weeks)
- Contrast enhancement slowly decreases in time but can persist for eight weeks, with decreasing mass effect.
Old Infarct:
- Focal area of encephalomalacia
- Porencephalic dilatation of adjacent ventricle
- Residual old blood products may persist.
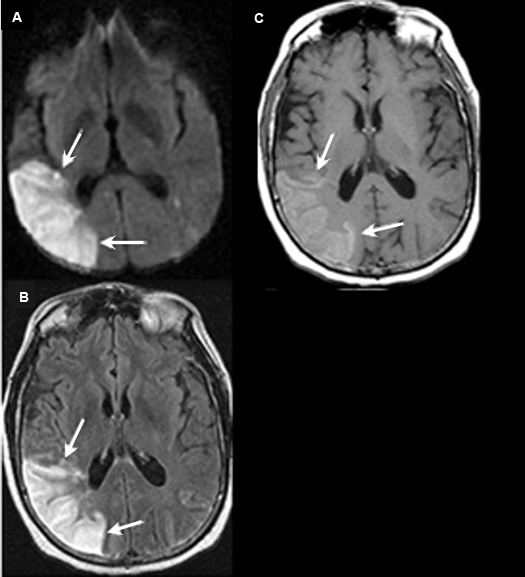
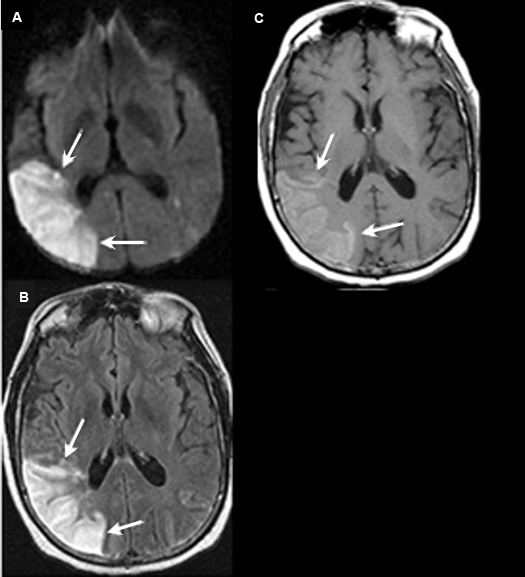
Figure 7: MR Images
|
Three Week Old Subacute to Chronic Infarction Involving the Right Middle Cerebral Artery Territory with Reperfusion Hemorrhage
Case 7:
Imaging findings: Figure 7
- Diffusion weighted image reveals bright signal involving the cortex (white arrows). This is from restricted diffusion secondary to acute infarction.
- Axial flair shows increased signal involving the posterior temporoparietal cortex with gyral thickening (white arrows).
- Pre-contrast axial T1 wtd. MRI shows increased signal (white arrows) in the same area from subacute blood in the distribution of infarct.
|
Q8: How does information gathered from imaging influence clinical management?
The goal of imaging in a patient with acute stroke is to determine:
- Is there an infarct?
- If there is an infarct, is it associated with hemorrhage? Thrombolytic therapy is then contraindicated.
- If there is an infarct, is there reversibly impaired brain tissue that could benefit from thrombolytic therapy?
- Nature of vascular abnormality? Is the abnormality in extracranial arteries or intracranial arteries?
Is there an infarct?
- Diffusion weighted imaging is the most sensitive sequence for stroke imaging. Bright signal is due to restriction of the ability of water protons to diffuse extracellularly.
- CT can be normal in acute stroke.
If there is an infarct, is it associated with hemorrhage?
- Hemorrhage is best detected by CT and is a contraindication for thrombolytic therapy.
If there is an ischemic infarct, is there reversibly impaired brain tissue?
- Thrombolytic therapy utilized only if there is reversibly impaired brain tissue.
- Combining perfusion and diffusion image helps us to define the tissue at risk (penumbra).
- Diffusion image indicates dead tissue. Subtracting diffusion image from perfusion indicates tissue at risk which can be saved with therapy.
- If diffusion and perfusion images match, no thrombolytic therapy is needed.
- When there is mismatch between perfusion and diffusion images, patient is a candidate for therapy.
Nature of vascular abnormality? Options to investigate?
- Is the primary abnormality in extracranial arteries or intracranial arteries?
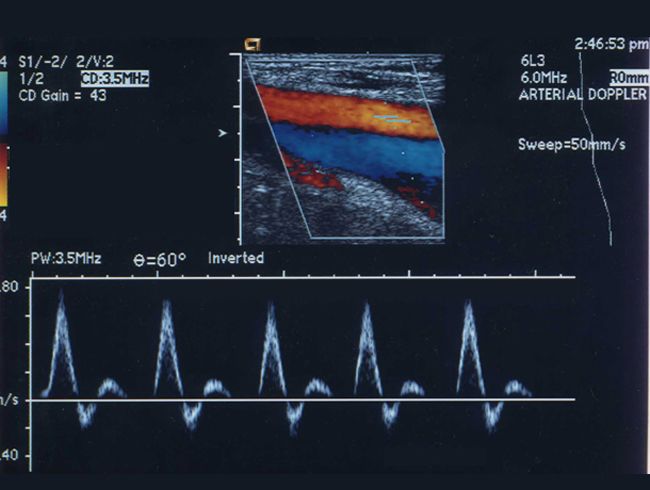
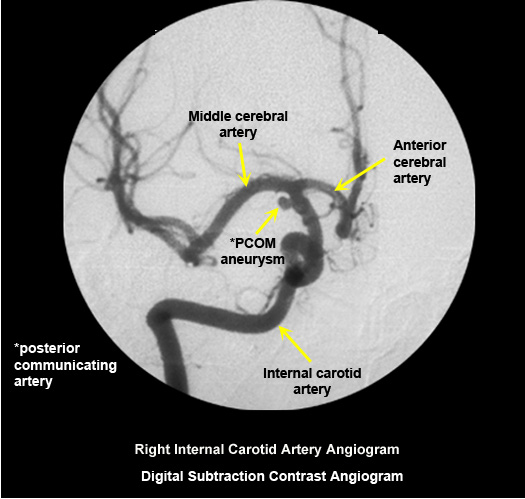
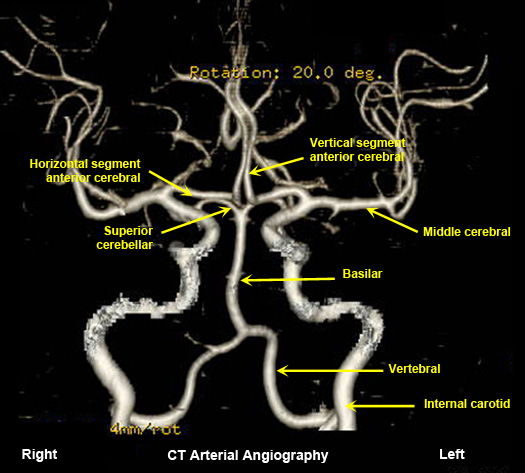
- Doppler US is the least expensive study to evaluate carotid bifurcations. MR angiogram and CT angiogram are non-invasive studies to investigate extra and intracranial arteries. Digital subtraction intra-arterial contrast angiogram (DSA) is invasive and definitive. If interventional therapy is contemplated, such as retrieval of clot from major arteries one needs to do dedicated invasive digital subtraction contrast angiogram.
|
US of carotids
No radiation |
|
Normal digital subtraction contrast angiogram
Arterial puncture required.
Selective intra arterial contrast injection into right internal carotid artery. |
|
Normal CT arterial angiography
Contrast administered intravenously. |
|
Normal MR arterial angiography
No radiation.
Contraindicated when there are metallic objects in the critical sites. |
When you interpret imaging studies during your clerkship, I want you to make the following statements:
- Is it hemorrhagic infarct or non-hemorrhagic infarct? Obviously anticoagulation or thrombolytic therapy is contraindicated in hemorrhagic infarct. If it is hemorrhagic, assess extension into ventricles.
- Decide on which vascular territory: anterior, middle, posterior cerebral artery?
- Is it acute, subacute or chronic? DWI is most valuable for this purpose.
- Is there reversibly impaired brain tissue? At this stage of learning, you need not worry about this. For this you need to understand perfusion and diffusion imaging. Thrombolytic therapy is not useful if there is no reversibly impaired brain tissue.
- Are there signs of mass effect due to edema and hemorrhage? Look for effacement of gyri and sulci, compression of ventricles, etc.
- Is the stroke due to intracranial vascular disease or due to extracranial vascular disease? You will need history and other clinical information to make this assessment. This will help guide in further work-up.
|