Pericardial Effusion
How do you distinguish cardiomegaly from pericardial effusion?
- There is pulmonary congestion in CHF and pulmonary oligemia in pericardial effusion.
- Shape of the heart is helpful
- Water bottle appearance in pericardial effusion.
- Displacement of precardiac fat line in pericardial effusion .
What are the Common Causes for pericardial effusion?
- Idiopathic
- Infection
- Autoimmune (SLE, rheumatoid arthritis, scleroderma)
- Dressler's and postpericardiotomy syndromes
- Neoplasm (lymphoma, lung or breast metastasis)
- Drug-induced (procainamide, hydralazine, phenytoin)
- Uremia
- Myxedema
- Congestive heart failure
- Trauma
How would you evaluate a patient suspected to have pericardial effusion by Imaging studies?
CXR, US, CT amd MR have roles in the evaluation of pericardial effusion.
CXR:
In patients with a large pericardial effusion (at least 250 ml), the chest radiograph usually demonstrates
- Symmetrically enlarged cardiopericardial silhouette.
- The appearance has been characterized as the �flask� or �water bottle� configuration.
- The normal great vessels contours are smoothed out and the hilar vessels are obliterated.
- The cardiophrenic angles show acute rather than obtuse angles.
- On the lateral view there may be loss of retrosternal �clear space�.
- Another clue is the rapid change in heart size or presence of cardiomegaly without the radiographic findings of congestive heart failure (pulmonary edema, etc.)
- Posterior displacement of epicardial fat pad by effusion.
- Pulmonary olegemia.
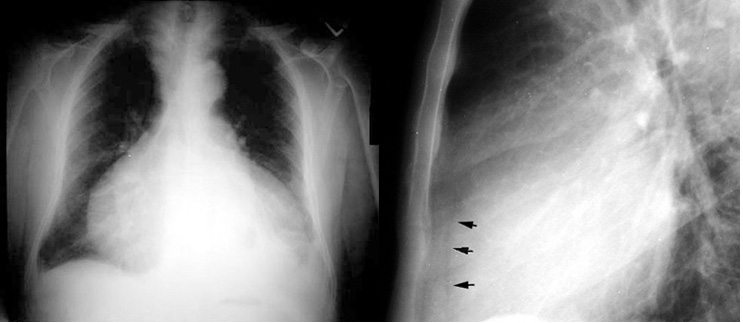 |
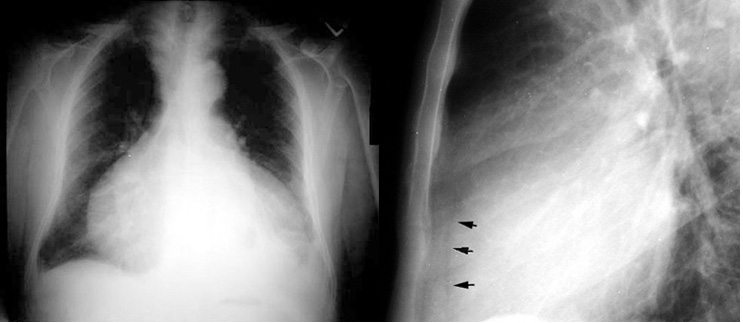
Enlarged cardiac silhouette could be pericardial effusion or cardiac enlargement. Lateral chest radiograph shows sign indicating effusion. Dorsally displaced epicardial fat pad (arrows) indicates that the cardiac silhouette is due to pericardial effusion.
|
3D Echocardiography: is the radiologic modality of choice for evaluating pericardial effusions.
 |
Pericardial Effusion
Echocardiogram showing fluid surrounding the heart.
|
- If performed in patients with good acoustic windows, echocardiography will accurately detect all pericardial effusions and provide important information about their size and hemodynamic importance.
- Echocardiography is less reliable than MRI or CT in detecting pericardial thickening or small loculated effusions, but it is still extremely useful in these conditions.
- Echo free space around heart.
- Accumulation of pericardial fluid creates an anechoic space between the posterior left ventricular wall and the anterior parietal pericardium. In larger effusions, a similar echo-free space exists between the anterior right ventricular wall and the anterior parietal pericardium and chest wall.
- The technique is semi quantitative: very small effusions (50 -100 ml) are imaged only posteriorly, with separation of pericardial and epicardial echoes only in systole; small to moderate effusions (100 - 300 ml) are imaged only posteriorly throughout the cardiac cycle; and large effusions (300 ml) are imaged both anteriorly and posteriorly. Because of the oblique pericardial sinus, the echo-free space disappears behind the left atrium unless massive pericardial effusion is present.
- Diastolic collapse of right ventricle.
- Dilated inferior vena cava.
Case of cardiac tamponade:
CT : is valuable for detecting loculated pericardial effusions and in detecting pericardial thickening
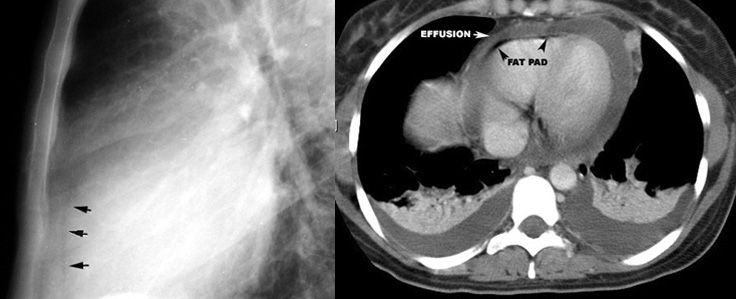 |
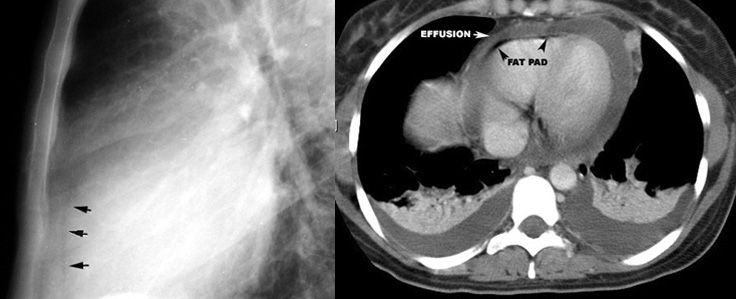
Epicardial fat pad is displaced posteriorly by pericardial effusion. Low density fluid density around heart.
|
MRI
- may be able to characterize the fluid as serous or hemorrhagic (because of characteristic changes in signal intensity).