Pulmonary emboli
What are the risk factors for pulmonary embolus?
- birth controll pills
- immobilization
- surgery within the last three months
- history of previous venous thromboembolism
- malignancy.
What are the imaging procedures available to investigate PE?
There are several modalities of imaging available to investigate PE
- Chest x-ray
- V/Q scan
- Helical CT scanning
- Non invasive lower extremity dopplers with compression US.
- Pulmonary angiography
- Echocardiography
What is the utility of each?
- Chest x-ray: Initial imaging procedure. It is either normal or non specific in most of the patients. Needed to correlate with V/Q scan. Useful to exclude other conditions that simulate PE.
- V/Q scan - a commonly used study because a normal perfusion scan virtually excludes the diagnosis of pulmonary embolus. A high probability lung scan indicates a high likelihood of emboli, particularly in patients with a high pretest probability.
- Helical CT scanning ; is competing with V/Q scan as the initial procedure for the diagnosis of pulmonary embolism. Concern regarding sensitivity for smaller and peripheral emboli.
- Non-invasive lower extremity dopplers ; has some utility in the evaluation of patients with intermediate clinical and scan probabilities for pulmonary emboli. Positive results would indicate anticoagulant therapy. Negative results will not rule out PE.
- Pulmonary angiography ; Very rarely used nowadays. It used to be the gold standard. CT angiogram has replaced the need for angiogram.
- Echocardiography ; generally has a low sensitivity for diagnosing pulmonary embolism, but may be useful in cases of massive PE where a rapid presumptive diagnosis is required to justify the use of thrombolytic therapy
- Case 1 : Massive pulmonary embolus
- Case 2: Thrombus in the right pulmonary artery.
What is the appropriate sequence of imaging procedures?
Two options:
- CXR followed by Helical CT
- CXR, V/Q scan. If V/Q scan is equivocal Helical CT.
Describe the mechanism and limitation of VQ scan?
Concurrent images of the distribution of blood flow (perfusion scan) and the distribution of alveolar ventilation (ventilation scan) are obtained following the intravenous injection of 99m Tc-labelled particles of macroaggregated albumin, and the inhalation of a radioactive gas (for example, krypton-81 m or xenon-133) or -carbon particles known as �Technegas'.
Typically in PE, the perfusion scan shows segmental perfusion defects, while the ventilation scan remains normal, the so-called �mismatched perfusion defect'.
A properly performed perfusion scan, which includes at least six projections, is highly sensitive for the detection of small defects. However, this high sensitivity is not matched by a high specificity for the diagnosis of pulmonary embolism. There are many causes of positive perfusion scans, which could lead to a false positive diagnosis of pulmonary embolism. Various conditions can cause mismatched defects on ventilation-perfusion scanning including emphysema, tuberculosis, previous irradiation etc.
What is the need for baseline CXR for lung scan?
- For the reasons given above, it is helpful to have a baseline CXR to evaluate the patient for the underlying presence of COPD, or other conditions, which could complicate the lung scan and lead to a false positive diagnosis.
What do you understand from the terms normal, high probability and low probability scans?
- A normal perfusion scan virtually excluded the diagnosis of pulmonary embolus.
- A high probability lung scan indicated a high likelihood of emboli, particularly in patients with a high pretest probability. The cardinal sign of pulmonary embolism is an underperfused part of the lungs on perfusion scanning. Typically the defect is segmental, while the ventilation scan remains normal, the so-called �mismatched perfusion defect'.
- Low probability scan when there is matching perfusion and ventilation defects.
- Indeterminate scan
Low probabilty and indeterminate scans do not rule out the possibility of PE. If there is a clinical suspicion for PE further studies should be done.
What is the sensitivity and specificity of lung scan in diagnosing PE?
- High probability lung scan indicated a high likelihood of emboli, particularly in patients with a high pretest probability- 95% specificity, however they were not very sensitive for PE, 42% sensitivity.
- Best estimates suggest that a normal ventilation-perfusion scan excludes pulmonary embolism with a probability approaching 95%.
What are the imaging findings of PE in CT angiogram?
|
CT Angiogram Showing Filling Defects Consistent With PE
Patient had a low probability lung scan. Clinically there was high index of suspicion for pulmonary embolism.
Arrowheads: Intra luminal thrombi in right pulmonary artery branches |
|
|
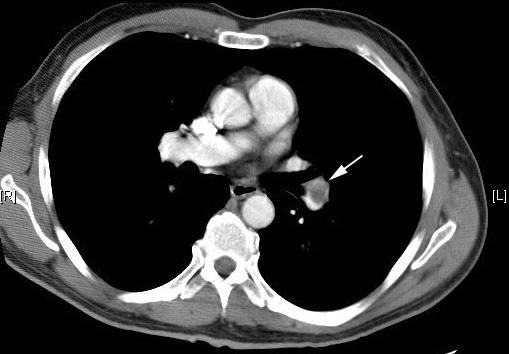
Pulmonary Embolus
Arrow: Filling defect in pulmonary artery. |
|
What is the sensitivity and specificity of CT?
- The sensitivity in studies has ranged from 53-87%, and the specificity is generally regarded as being above 90%, although reader experience appears to be necessary to avoid false positive results.
What is the role of Doppler exam?
- Noninvasive assessment for deep venous thrombosis may be helpful in the evaluation of patients with intermediate clinical and scan probabilities for pulmonary emboli.
- Compared to venography, color-flow Doppler with compression ultrasound has high sensitivity (89 to 100 percent) and specificity (89 to 100 percent) for the detection of a first episode of proximal venous thrombosis.
- Venous ultrasound is less sensitive when evaluated in high-risk asymptomatic patients (as low as 38 percent sensitivity and 26 percent positive predictive value).
What is the role of pulmonary angiogram in evaluating PE?
- Pulmonary angiogram used to be the gold standard in this disease, and is performed by injecting iodinated contrast into a pulmonary artery branch after percutaneous catheterization.
- Spiral CT angiogram has practically replaced the need for angiogram and is rarely done.